Skepticism and resistance

With the rapidly developing digital landscape, new technologies can appear unfamiliar and instigate a feeling of uncertainty. Skepticism and resistance are common human emotions, that can be triggered when introducing new technology. This module will present you with some insights into why skepticism may arise and how to handle it.
The interaction of technology and humans
Many times, and in particular in the healthcare system, new technology is met with skepticism and resistance. This may be due to the fact that wrongful use of technology may potentially harm patients and their wellbeing. It may also be due to psychological factors (see part about: Motivation of the healthcare professional).
However, many of the technologies that are currently being used in the daily work lives were at some point in time new. Over time, they have been incorporated into the work place and the use of them has become natural routine.
As a healthcare manager, it is important to acknowledge the different ways we interact and react to technology. In particular when the technology is met with resistance and skepticism. This counts for both healthcare professionals and patients.
However, it is important to keep in mind, that healthcare technology is constructed through interaction with the world around it. There is no inherent value or intention of a technology. Instead, it is humans who give meaning to a certain technology through their use of it.
Source / References
- Botin, L., Bertelsen, P. S., Kayser, L., Turner, P., Villumsen, S., & Nøhr, C. (2020). People Centeredness, Chronic Conditions and Diversity Sensitive eHealth: Exploring Emancipation of the ‘Health Care System’and the ‘Patient’in Health Informatics. Life, 10(12), 329.)
- Resistance – (Bauer 1995, 16, 18)
- https://www.sciencedirect.com/science/article/pii/S0277953613003304 Greenhalgh et al. (2013)
- Lapointe, Liette and Suzanne Rivard. 2005. “A Multilevel Model of Resistance to
- Information Technology Implementation.” MIS Quarterly 29 (3): 461–91. DOI: 10.2307/25148692
Users and non-users

When implementing a technology, non-users are created unintentionally. While users can be important, this module will primarily focus on non-users, since they are often overlooked in the development and implementation phase of a new technology.
Users are those who use the technology.
Non-users are those who do not use the technology – or do not use it as intended.
Healthcare professionals as well as patients can exist in both groups.
This section introduces an understanding of the different natures of non-users and their behavior.
While users are important, this module will primarily focus on non-users, since they are often overlooked in the development and implementation phase of a new technology.
The forgotten
When implementing a new technology resistance may occur. Resistance can be understood in terms of active or passive resistance, and in terms of individual action or collective action. The level of intensity with which the resistance occurs may also vary.
Some people might be more skeptical of technology than others. However, non-users may be created when a certain group feels marginalized or “forgotten” in the development- or implementation phase. The creation of non-users might also take place when new technology is experienced as problematic in terms of both psychological safety and ethics.
Non-users are important stakeholders who can affect the process by shaping the network of technology and people necessary for healthcare technology to be successful. Therefore, there is a need to be observant and responsive to the needs of both users and non-users.
Source / References
- Botin, L., Bertelsen, P. S., Kayser, L., Turner, P., Villumsen, S., & Nøhr, C. (2020). People Centeredness, Chronic Conditions and Diversity Sensitive eHealth: Exploring Emancipation of the ‘Health Care System’and the ‘Patient’in Health Informatics. Life, 10(12), 329.)
- Resistance – (Bauer 1995, 16, 18)
- https://www.sciencedirect.com/science/article/pii/S0277953613003304 Greenhalgh et al. (2013)
- Lapointe, Liette and Suzanne Rivard. 2005. “A Multilevel Model of Resistance to
- Information Technology Implementation.” MIS Quarterly 29 (3): 461–91. DOI: 10.2307/25148692
The power of non-users

In an implementation project in Norway, the power of non-users was studied. In the project a large group of non-users were created and their large resistance of made the implementation of a health information system fail. The study identified four archetypes of non-users.
In a study of an implementation project in Norway, the power of non-users is evident. In the study a large group of non-users were created. The resistance of the non-users makes the implementation of a health information system fail.
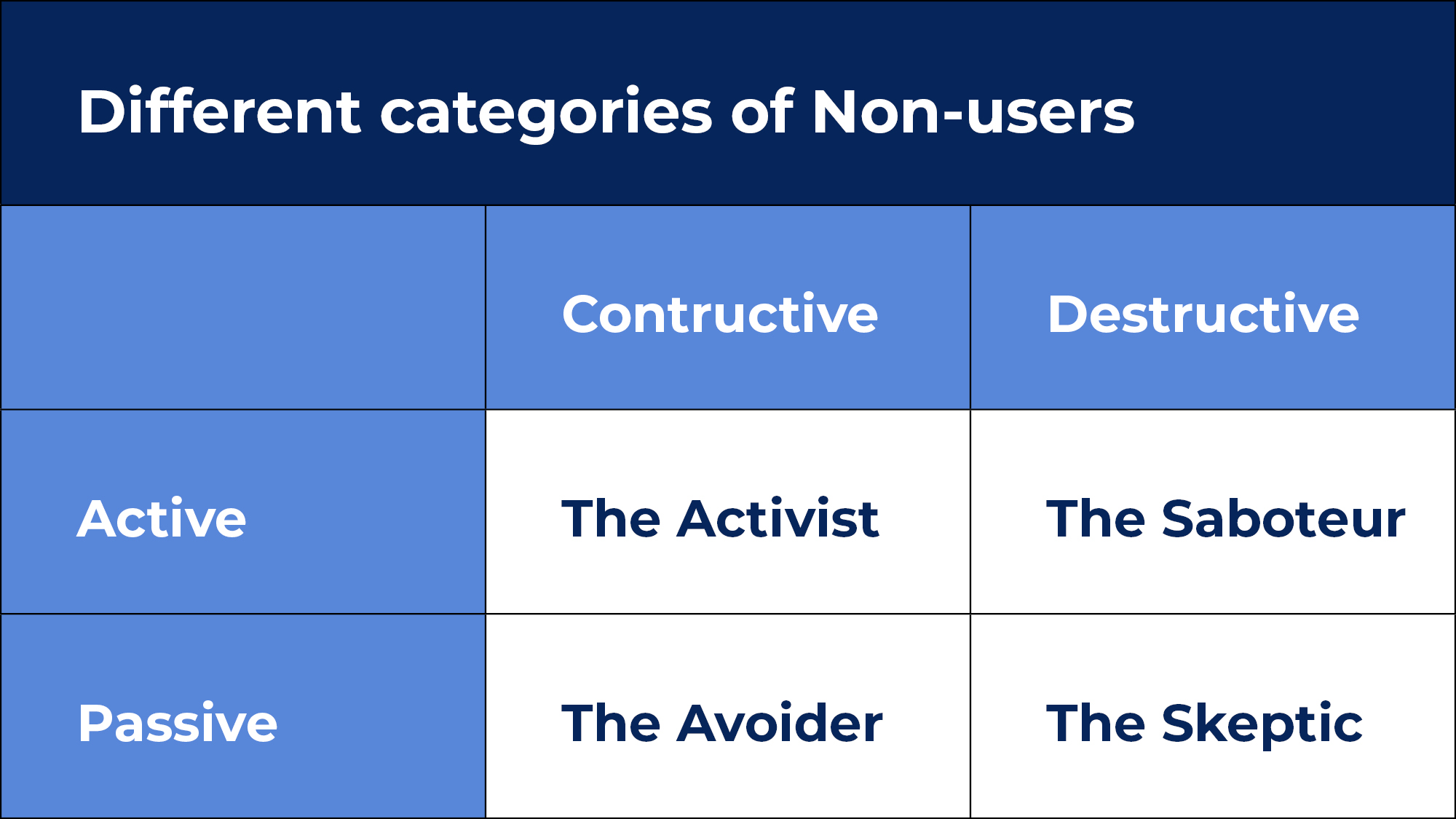
The study categorizes four archetypes of non-users on two dimensions:
An active/passive dimension – referring to whether or not the actor takes active measures in expressing resistance.
Constructive/destructive dimension – referring to the overall attitude towards the system and actual use; how potential users perceive the usefulness of the system.
The four archetypes of non-users
The Activist: The activist is an active and constructive actor who has knowledge enough about the system to provide constructive criticism. They are valuable, in the sense that they can provide constructive feedback.
The Saboteur: The saboteur is actively participating in hindering the implementation process by refusing to participate in the training set in place for successful system use. They actively try to disintegrate the implementation network.
The Avoider: The avoider applies a passive strategy and is not engaged in meetings, and does not speak up to influence the implementation process. Will stick to old work routines and are just doing “their job”. The avoider is usually the biggest non-user group and as such can have a huge impact on the implementation success.
The Skeptic: The skeptic is characterized by a skepticism towards the intention of the implementation team, the managers and the overall usefulness of the system itself. The skeptic keeps a low profile and is not actively voicing skepticism and discontent to the managers.
Source / References
- Melby, L., & Toussaint, P. (2016). “We walk straight past the screens”: The Power of the Non-Users of a Hospital Information System. In The New Production of Users (pp. 249-272). Routledge
How to learn from non-users

Both user and non-user groups are crucial in the implementation process. Both groups can have eligible arguments and perspectives worth considering to achieve a sustainable implementation of a given technology.
In cases where the implementation process isn’t going as planned, the user group might not be the most suitable for articulating why the technology isn’t being used. In this case it might be necessary to examine the non-users.
In particular constructive non-users can lead to crucial insights in understanding why the implementation process has come to a halt. They critique the system by identifying features that would make the system acceptable to the other non-users. They are often willing to use the system if it meets their demands.
Destructive non-users are more difficult to engage – in particular the saboteur. However, they can still lead to valuable insights – since the strong emotional response has been triggered, but common ground can be difficult to establish.
Source / References
- Botin, L., Bertelsen, P. S., Kayser, L., Turner, P., Villumsen, S., & Nøhr, C. (2020). People Centeredness, Chronic Conditions and Diversity Sensitive eHealth: Exploring Emancipation of the ‘Health Care System’and the ‘Patient’ in Health Informatics. Life, 10(12), 329.)
- Resistance – (Bauer 1995, 16, 18)
- https://www.sciencedirect.com/science/article/pii/S0277953613003304 Greenhalgh et al. (2013)
- Lapointe, Liette and Suzanne Rivard. 2005. “A Multilevel Model of Resistance to
- Information Technology Implementation.” MIS Quarterly 29 (3): 461–91. DOI: 10.2307/25148692
Two methods of engaging non-users
To overcome a potential implementation deadlock Melby and Toussaint recommend the following:
Meetings and interviews: Scheduled meetings and interviews with the non-user group with the purpose of finding the reason why they refrain from using the technology. The list should be studied, addressed and accommodated as much as possible (Lapointe and Rivard 2005).
Study non-users and their behavior: The saboteurs and the avoiders are per definition difficult to engage or involve. Even if meetings are scheduled, they might not be willing to actively participate, and as such they are difficult to accommodate, since their worries and demands are unknown. In cases like this, ethnographic and observational studies can be an alternative method for insights.
Questions for reflection
- In which categories are the non-users of digital technology in our workplace?
- How can we engage the non-users in our workplace?
- What can we learn from the non-users in our workplace?”
What have we learned on managing the digital transformation?

Take home messages placed on ‘cards’ with questions for reflection on backside.
Healthcare managers play a crucial role in supporting healthcare professionals in embracing digital solutions. Based on this theme on how to support the digital health care professional, here are 8 important themes with questions for reflection which managers should consider to effectively support healthcare professionals overcoming resistance to change and actively participating in the digital transformation.
1. Prioritizing Training and Practice:
- How can we effectively integrate digital technology into our training programs to provide hands-on experiences for healthcare professionals?
- How can we identify and engage teachers who are specialized in delivering training on digital technology, such as external experts, dedicated training teams, or local frontrunners?
- How can we create opportunities for healthcare professionals to practice using digital solutions in their daily work?
2. Focus on Applicable Technology:
- How can we ensure that the digital technologies we provide training on are relevant and applicable to the healthcare professionals’ work?
- How can we prioritize fully developed and tested technologies that are reliable in the clinical setting?
3. Promoting Exploration and Reflection:
- How can we create a stress-free environment that encourages healthcare professionals to explore digital technology, learn from mistakes, and share their experiences?
- How can we promote reflection among healthcare professionals on the problems and advantages of digital technology for both patients and healthcare professionals?
4. Involvement of Healthcare Professionals and Citizens:
- How can we effectively listen to and incorporate the perspectives of healthcare professionals when making decisions related to digital solutions?
- How can we encourage healthcare professionals to involve citizens in discussions to gain a better understanding of their perspectives?
- How can we establish processes and structures that facilitate the sharing of experiences and knowledge among healthcare professionals?
5. Ensuring Accessibility, Support, and Guidance:
- How can we ensure that digital solutions are easily accessible and user-friendly for healthcare professionals?
- How can we provide convenient access to support systems, such as colleagues, local frontrunners, and ICT departments, for troubleshooting and guidance?
- How can we make sure that user guides and resources for digital solutions are readily available in the clinical setting?
6. Breaking Changes into Smaller Steps:
- How can we break down changes related to the digital transformation into smaller, manageable steps that align with existing workflows and habits?
- How can we consider the timing of change initiatives to avoid overwhelming healthcare professionals and promote smoother adaptation to new digital solutions?
7. Recognizing and Rewarding Progress:
- How can we provide positive feedback and recognition to healthcare professionals who make efforts to use digital solutions, even when they encounter challenges?
- How can we acknowledge the improvement and effort made by healthcare professionals, and provide ongoing support throughout the change process?
8. Clear Communication:
- How can we effectively communicate behavioral expectations and changes related to the digital transformation in a clear and practical manner?
- How can we avoid using ambiguous buzzwords and instead provide explanations and examples that directly relate to the healthcare professionals’ existing work practices?



