A model for employees’ reflections on use of technology

This model is intended for healthcare professionals to reflect on their use of technology in working life. It is a reflection tool for enabling active use of technology.
Introduction to the model
Too often healthcare professionals simply use technology routinely, even if it is not meaningful. This we can call passive use of technology, where the technology is used unreflectedly. Healthcare professionals may also refrain from using technology because they have not been able to reflect on the possibilities of use.
When the healthcare professionals, on the other hand, actively reflect on the use of technology, there is a much better chance that the technology is used in ways that best promotes clinical purposes.
Active reflection on the use of technology is thus essentialt to successful implementation of the solution.
Here is a model for healthcare professionals to reflect on their use of technology in their working life.
The model offers a common language to understand and talk about technology in working life.
The model is used by Copenhagen University of Applied Sciences for digital competence development of healthcare professionals.
Elements in the model
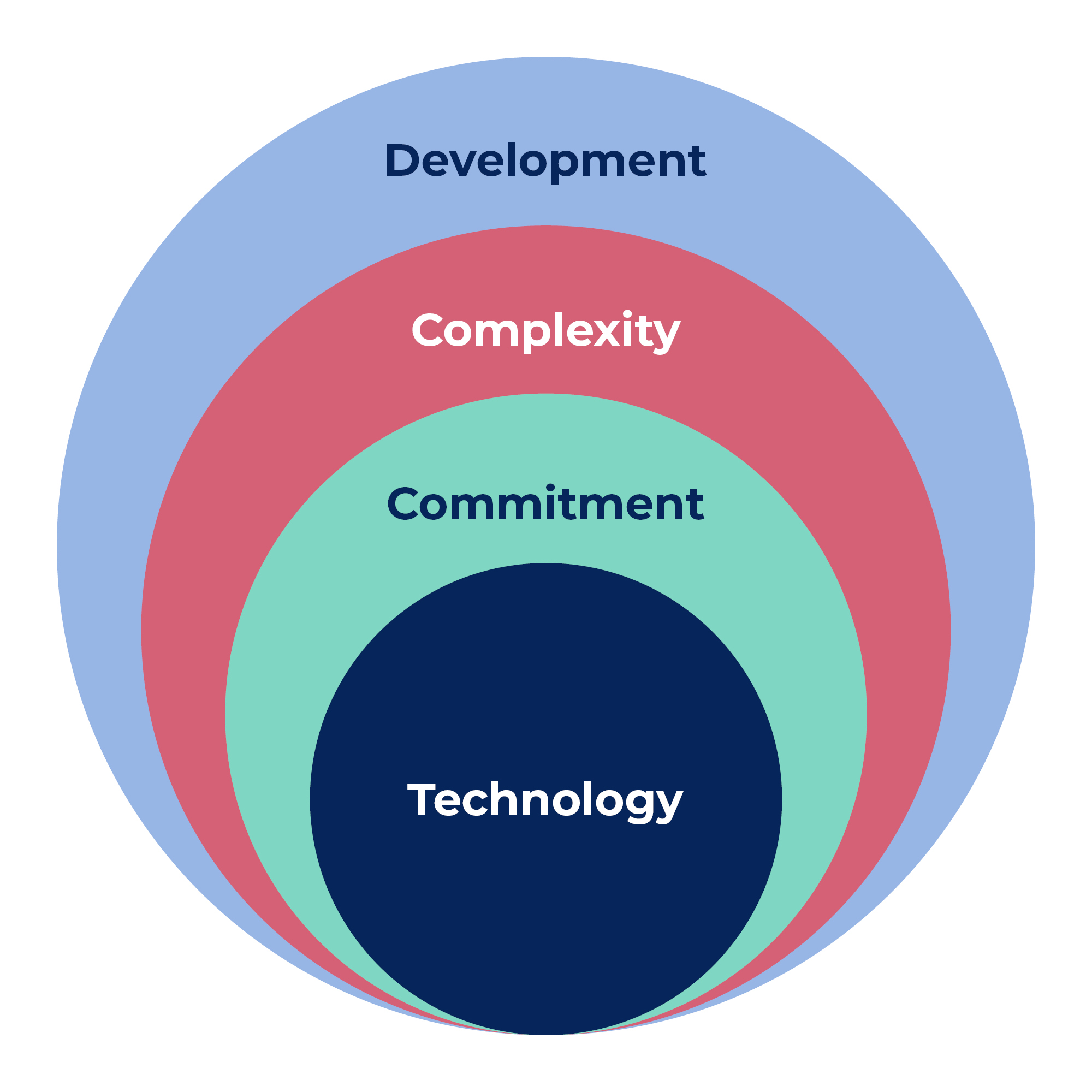
The model consists of four dimensions of technological understanding, which are important for the health care professionals to reflect on when introduced to new digital technologies at work. These dimensions are:
- Technology – touching upon the learning requirements of new technological solutions
- Commitment – to learning new technology in work life
- Complexity – regarding the complex contexts in which the use of technology takes place
- Development – about the changes in professional identity that new technology entails and the needs for rethinking and development.
Sources / References
- Hasse and Brok, 2015: TEKU – modellen – Teknologiforståelse I professionerne
Exercise
How to use the model:
Use 30 minutes in smaller groups to reflect on how you use technology in your everyday work. Apply the questions why, how, who and what to guide the dialogue.
Reflections on technology use

Development
- How am I affected as a healthcare professional?
- How does the technology influence on/develop my professionalism (influences working methods, professional expertise and professionalism)?
- Which new tasks does the technology create? And how does the organization of the tasks change?
- How are responsibility and trust in relationships affected? As well as hierarchies and knowledge monopolies and forms of collaboration across the board?
Complexity
- Why is this technology introduced? (Decision from management, employees or political and with what intent and purpose?)
Commitment
The impact of technology on everyday life:
- How does this technology change my specific work tasks? (new interior design, new workflows, new form of communication, new approach to the patient – new habits and routines)
The way technology is used in practice:
- Have we taken an active position on how we use technology most meaningfully?
- Does the technology even make sense?
- When is the use of digital technology problematic and when is it beneficial?
- How does technology affect my relationship with the patient?
- What ethical questions arise when we use this technology? And in what situations?
- How does technology affect the quality of treatment/care? Including how we handle challenges such as crashes, many codes, etc.?
Technology
- How do I get to know the technology and become able to use it in my everyday life?
- How do my own attitudes and feelings affect the way I approach new technology?
- What motivates me to acquire new technology?
Source / References
- Hasse, C., & Brok, L. (2015). TEKU – The TEKU Model – Technological Understanding in the Professions.
Dialogue cards for reflections on technology and its effect in practice

The use of digital technology in healthcare requires several important considerations. In the following you will be presented with a set of dialogue cards related to the use of technology in healthcare. Use these cards to reflect and discuss.
Cards for dialogue and joint reflection
It is important that you have a common language in your workplace to talk about digital competencies. You can strengthen this by using the dialogue cards to talk about where you encounter digitalization and what it requires of you.
Source / References
- Dialogue cards – KL kompetencehjuletLink (in Danish):https://videncenter.kl.dk/media/7932/dialogkort-medarbejdere-digitale-kompetencer.pdfMachine translated by Google. Edited by Syddansk Sundhedsinnovation
How to use the dialogue cards
Print the cards where your print on both sides of the paper. The dialogue cards can be used in a group or on your own.
They contain questions about four areas:
- Application competencies
- Technology understanding
- Communication
- Development and implementation
- Dialogue cards
Process tools

Which tools could I as a health care professional or manager use to assess and train the use of digital technologies as well as reflect on how to implement digital solutions?
On the website provided by the project DISH (Digital and Innovation Skills Helix in Healthcare) you will find process tools for:
- Planning and Implementation
- On-the-Job Training
- Assessment and Recognition
The website also contains case studies that provide insight as to how to apply the tools in practice.
The website offers a platform for continuous professional development and focuses on areas such as digital communication, data management, telemedicine, remote monitoring, and health technology assessment.
The DISH project is another program aimed at enhancing the digital competencies of healthcare professionals and co-funded by the Erasmus+ Programme of the European Union.
Find the website here: Homepage – Dish Project
Case-example: The digital healthcare professional

To give you an example of how being a digital healthcare professional may look in practice we have provided you with a case-example. The case is quite idealized as the health care professional no longer faces any problems.
Sarah is a healthcare professional working in a primary care clinic. Over the past few years, she has witnessed the increasing digitalization of the healthcare system and has actively embraced various digital tools and technologies to improve patient care.
Sarah has noticed a significant shift in her daily routines. Previously, she relied heavily on paper-based records and manual documentation. However, with the implementation of electronic health records (EHRs) and digital charting systems, she now spends less time on paperwork and has quick access to patient information, allowing her to provide more efficient and informed care.
Sarah has integrated several digital tools into her practice. For instance, she uses telemedicine platforms to conduct virtual consultations, which has increased accessibility for patients who have difficulty visiting the clinic physically. Additionally, she encourages patients to utilize mobile health apps and wearable devices to monitor their vital signs, track their medications, and engage in self-management. These tools have improved patient engagement, empowered individuals to take control of their health, and facilitated better communication between Sarah and her patients.
With the digitalization of healthcare, Sarah has taken on new roles and responsibilities. She now acts as a health coach, guiding patients through the abundance of health information available online and helping them navigate the “information jungle”. Additionally, she has become proficient in using digital communication platforms to interact with patients, collaborate with other healthcare providers, and coordinate care across different settings.
Sarah recognizes the importance of maintaining a human connection with her patients despite the increased use of digital technology. She ensures that virtual consultations are conducted in a patient-centered manner, actively listening to their concerns, and addressing their emotional needs. She emphasizes the importance of regular in-person visits for establishing a strong rapport and builds trust by providing personalized care and being accessible for questions and support.
Sarah initially faced challenges in learning and adapting to new digital tools and systems. She attended training sessions and workshops to enhance her digital competencies. Additionally, she sought guidance from tech-savvy colleagues and engaged in online communities where healthcare professionals shared best practices. Over time, Sarah has become proficient in using digital tools and has found that ongoing learning and collaboration are effective strategies for managing the transition to a more digital healthcare system.
To stay updated, Sarah regularly attends conferences, webinars, and continuing education courses focused on digital healthcare and emerging technologies. She actively engages in professional networks, subscribes to relevant journals, and follows industry experts and thought leaders on social media platforms. Additionally, Sarah participates in research studies and pilot programs that explore the integration of innovative digital solutions into clinical practice.
Questions for reflection:
- In which areas does Sarahs working life resemble yours?
- Which parts of Sarahs working life appeal to you?
- Which parts of Sarah’s working life do you expect to see more of in your workplace?
Why user-centred approach to the technological development?

Healthcare professionals should and can be an important voice in the development and implementation of new digital technology. In the following, the user-centered approach will be introduced in particular focusing on the participation of health professionals and patients in the development and implementation of new digital healthcare solutions.
Healthcare professionals – an essential voice in developing and implementing new technology
User participation in development and innovation processes is here to stay – especially, since we see a growing number of successful examples showing the value of user participation and healthcare technology development going hand in hand. The benefit of the user participation is that users are often the key to changing clinical practice and the existing culture. The participation also often increases the satisfaction with the process and its results.
Additionally, healthcare professionals have crucial, first-hand knowledge and insights that are invaluable for shaping design criteria and developing ethical and responsible healthcare technology.
A user-centered approach to innovation
A user-centered approach to design and/or innovation puts the needs, wants, and limitations of users at the forefront. It involves understanding the perspectives of users, their goals, and how they interact with a product, service, or system.
Since the late 1970s the field of design, originally a craftsmanship, has been adopting and forming several sub-disciplines based on ‘user-centredness’; e.g., user-centred systems design, participatory design, interaction and experience design, all of which give a central role to end users, while each focuses on a specific (part of the) design process, within the so-called ‘fuzzy front-end’. Participatory design, in particular, has Scandinavian roots and derives from the strong labor union movement. When applied in a project setting, participatory design assures that the user is not only a participant but becomes a co-designer. All design sub-disciplines, under the umbrella term ‘user-centred design approaches’, draw on common design methods but also methods and theories from the humanities e.g., anthropology, psychology and sociology.
A user-centered design process is a collaborative, iterative and reflexive process. The process often includes the following phases: empathy building, research, analysis, idea generation and conceptualization, prototyping and testing. In this context we have included the phases vision/plan, implementation and evaluation as they are essential for the planning of a project and successful implementation of new solutions. Continuous user participation is critical throughout the different phases.
The goal of a user-centred approach to innovative design is to create new products, services, workflows etc. that are easy to use/apply, intuitive, and meet users’ needs – and most importantly are meaningful. User-centred design has further been proven to increase user satisfaction, user engagement, and product adoption rates; meaning, that innovative solutions are also more likely to be implemented directly in e.g., clinical practice.
Important principles in a user-centered design process are mutual respect for each other’s knowledge and a commitment to facilitate genuine user participation, so that their voices and ideas directly influence the product and/or service design that will affect their lives.
Source / References
- https://dk/en/about-us
- An Introduction to Design Thinking Process Guide, Standford d.school, link: pdf (stanford.edu)
- Bødker, S. & O. Iversen, 2002. Staging a professional participatory design practice. NordiCHI ’02: Proceedings of the second Nordic conference on Human-computer interaction.
- Høy-Biegel, R. (2009). User-Driven Innovation: The Toolbox of the Innovation Architect. Changepilot, Aarhus.
Questions for reflection
- Are there digital solutions in your clinical practice that are not used in valuable and meaningful ways and that might create more value if used better/differently?
- Who are users or potential users of the solution, and who are key stakeholders when it comes to changing how the solution is used?
- From your standpoint/area of expertise, how do you reckon that involving and having health care professionals participate in technological development could be beneficial? Be specific.
- How could the participatory process be staged?
- How could you imagine having citizens participate in the development process of new digital healthcare technology?
How to use a user-centred approach to the technological development?

Vision and plan
When starting a user-centered process/project with focus on developing meaningful products or services or implementing existing ones, there are several important considerations:
- WHY is it important to start the project (which value do we hope to create for whom)?
- WHAT goals do we hope to achieve?
- HOW should we achieve them (time, resources and project plan)? How can we measure or evaluate the progress?
- WHO are the most important stakeholders, which roles should they have in the project and how should they cooperate? The stakeholders could, for example, be patients, relatives, health care professionals, designers, IT experts, researchers and others relevant to the project. It is critical to invite them to participate from the beginning of the project to clarify these questions. (Read more in the theme ‘Support the Digital Healthcare Professional’)
Research and analysis
To understand where in particular, digital technologies might be helpful and add value as well as where digital technologies are not the best solution, it is important to start with focusing on the needs of the users instead of focusing on the technology.
The users can be – and often are – both the health care professionals, patients and relatives. Where do they have challenges and unmet needs? Be curious, ask questions and observe interactions, workflows and the actual context in which users are situated in (see the tools ‘User Journey game’ and ‘Ask the citizen’ in the module ‘Tools for match-making’ in the theme ‘Match between technology and citizen’).
Following a qualitative research approach, one is able to be part of and engage in the users’ lives. It enables one to uncover both users’ expressed and latent needs (needs, which the users are not able to express or are unaware of).
Mapping existing knowledge in the area of interest through secondary research (e.g. literature studies), supplemented by e.g., expert interviews, is also an important part of this phase.
Ideation and conceptualization
Once the needs are identified it is possible to initiate the development of a potential technological solution which could meet the users’ needs. IT experts, coming from e.g., a private company or IT-department in a public organization, play a significant part in this phase. But ongoing dialogue and exchange of ideas through co-analysis and -design sessions between developers and users/users’ representatives are crucial to reach a solution that is valuable in the clinical practice and for citizens.
If a digital solution is already decided upon, the important focus in this phase is to explore how the digital solution could be used as well as ways of implementing the solution in detail, so that it best reflects the users’ needs, knowledge and expectations.
Through e.g., ideation workshops users can be involved in creating the solution, new concepts and/or prototypes to be tested. Some interesting questions to consider are:
- What are the expectations and ideas of the users/stakeholders?
- How do they suggest that digital solutions can be used (possible use scenarios)?
- How can the solution become an integral part of their daily lives?
- How can they learn, adjust and use the technology?
- What are possible improvements?
- Which user needs can, or cannot, be met?
Test and qualification
In this phase the solution is tested and qualified by the different users.
When cooperating with IT experts on developing a new solution, the test of the solution is often the responsibility of the IT company. But in order to create a user-centred solution it is important that the relevant users, e.g., health care professionals, patients and relatives, are deeply involved in iteratively testing and qualifying the solution.
When the project aim is not development of a solution but rather the successful implementation of a digital solution, the end product will probably be new workflows, new communication methods, new organizational setup etc. which also have to be tested.
In both cases the tasks in this phase are to; plan how to test the solution, actually test it in daily clinical practice, evaluate and adjust the solution after the test. Iteration is key here! Since one round of testing and qualifying often raises new questions, new research, analysis and ideation have to be done in the second round… and third round – and solutions have to be tested again, and again, until a fitting and user-centred solution is finally found.
Implementation and evaluation
Implementation must already be planned for at the beginning of the project. Make sure that both the intended users of the solution as well as all who are to facilitate the implementation of the solution are involved as soon as possible. Apart from health care professionals, patients and local IT experts, there might also be other key stakeholders such as colleagues from e.g., the communication department, building services or management. Also make sure to have a plan for evaluating the effects/benefits of the project; for instance, how many use the solution, how satisfied are the patients? Preferably measure several times and over many months after the project has ended to keep track of the changes.
It is a good idea to always keep in mind ”Hofstadters law”, when it comes to implementation:’It always takes longer than you think, even when you take this into account’. Implementation is often seen as obvious but not easy. We know what we have to do, but it is still difficult to get it done. By nature humans are creatures of habit and tend to save as much energy as possible. It is therefore hard work to orient oneself towards new knowledge and new ways of doing things, and actually change behavior and ingrown habits. It also demands that the initiater of the changes initiates and runs the right amount of activities to keep up the energy in the process. (Read more on implementation and changing behaviour and habits in the module ‘Supporting changes’ in the theme ‘Support the digital healthcare professional’)
Source / References
- Syddansk Sundhedsinnovation and Motivation of the healthcare professionals https://dkgl.dk/ressourcer/telesundhed/#/



