In the following 4 ethical dilemmas arising from the use of new technology are presented. The stories are based on specific situations. If the situations are not immediately recognizable to you, try to relate them to your own practice.
Dilemma: Home Measurement

Katrine is a nurse at the Heart Outpatient Clinic, where her task is, among other things, to follow up on the patients’ values and general well-being when they have been sent home after heart surgery.
Karl, a 72-year-old gentleman, underwent heart surgery two weeks ago. Today, he’s at the outpatient clinic for a follow-up appointment. His nurse, Katrine, notices immediately that Karl appears to be extremely anxious. During their conversation, Karl reveals that his grandson has helped him install several health monitoring apps on his smartphone so he can keep a closer eye on his vital statistics.
However, instead of providing reassurance, the apps have heightened Karl’s concerns. He’s noticed fluctuations in his blood pressure and pulse throughout the day, leading him to worry that the surgery hasn’t improved his condition. Consequently, he’s grown increasingly fatigued and despondent, confined to his home out of fear that he might collapse if he ventures too far.
Source / References
Questions for reflection
- What does the situation mean for the patient’s vulnerability or sense of security?
- Do you think that citizens should have full access to their own health data? Why/why not?
- Which – if any – responsibility do healthcare professionals bear in educating citizens about their own health data?
- How can the situation affect your daily workflow and task solving?

Dilemma: Night surveillance

Maria is healthcare social worker and works as a night watchman at a nursing home. Recently, the care home has installed a camera in Johannes’ room. Instead of Maria disturbing Johannes at night by opening the door and looking in on him, she can now take care of the night supervision virtually.
Maria can see on her screen whether Johannes is in bed. She doesn’t have to look all the time, but takes the agreed-upon looks several times during the night. Maria has heard from the day guards that Johannes has become healthier during the day after they introduced virtual night supervision. Maria also knows that in the past she often woke him up when she opened the door and looked in.
On the other hand, Maria feels a little strange about monitoring Johannes on a screen. She feels it is boundary crossing to look at someone who is sleeping, even though Johannes has given permission for the camera. Maria considers what she thinks about camera surveillance in general (e.g. in public spaces) and how her task here at the nursing home differs from it.
Source / References
Questions for reflection
Consider Maria’s situation of feeling that she is overstepping her own ethical boundaries simply by performing her work. What reflections do you have regarding this?
Should you disregard personal ethical boundaries in order to do your work? When – if ever – is a boundary okay to be disregarded?
How can the situation affect your daily workflow and task solving?

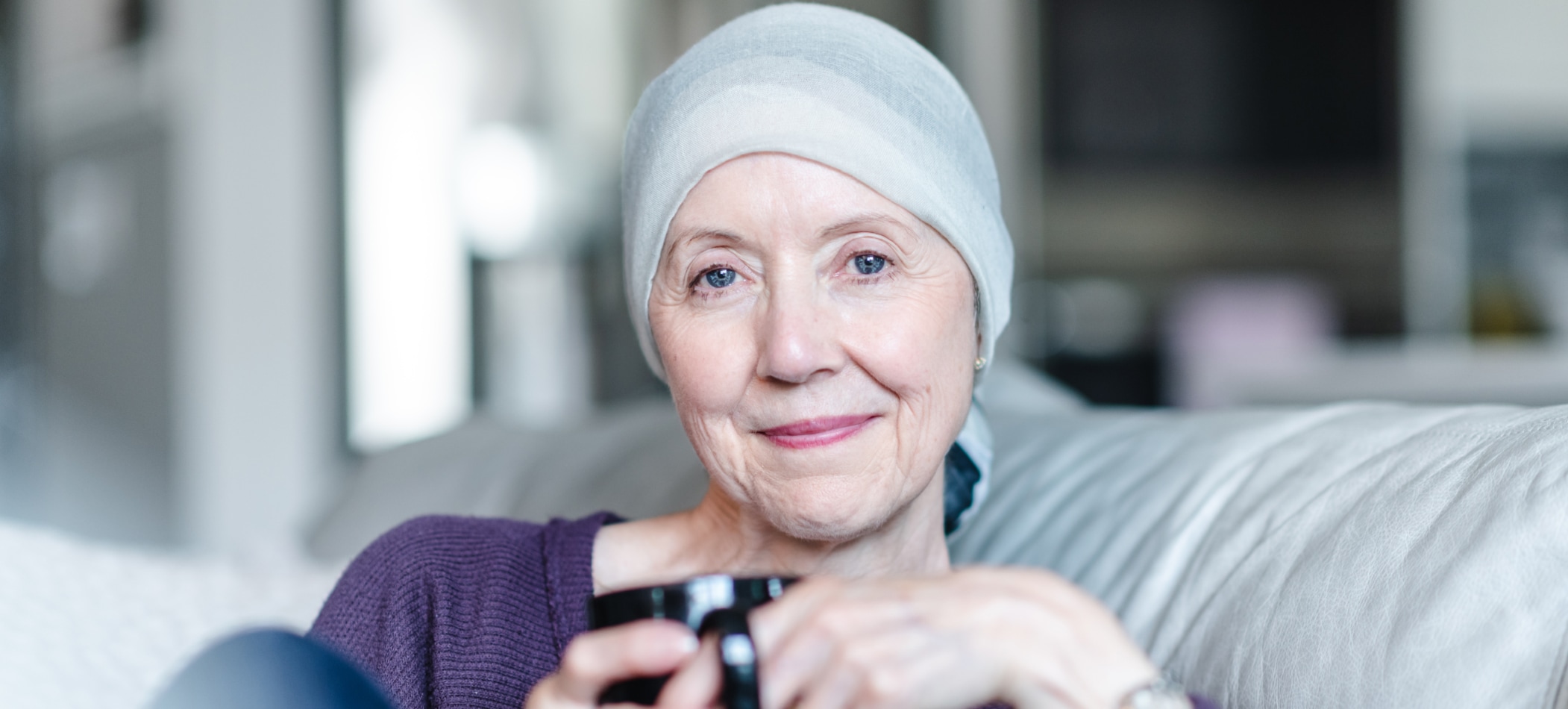
Dilemma: Breast screening

Fatima is a doctor in the oncology department, where, among other things, they work on automating X-rays from breast cancer screenings. Fatima uses a computer algorithm to help evaluate the many X-ray results. This means that a computer checks the images for irregularities and diagnoses through image recognition. In this way, Fatima and her colleagues can go through the images much faster.
Fatima can see that the use of computers will benefit many, as the patients get faster answers to their screening and therefore have a shorter waiting time before a possible treatment. However, Fatima is a little skeptical about a computer preparing decision support for health assessments. Wouldn’t it be safer with a personal and targeted medical assessment?
Fatima is worried that some patients will fail the algorithm and get a false-negative answer. They will then not be examined further by a doctor, even if they actually have symptoms of breast cancer.
Source / References
Questions for reflection
- Consider the ethical pros and cons regarding automation of processes in the healthcare system. Are they the same for the healthcare professional and the citizen? Where do they differ?
- How does the situation affect the trust and relation between the citizen and the healthcare professional?
- What does the situation mean for the patient’s vulnerability or sense of security?
- How can the situation affect your daily workflow and task solving?

Dilemma: Net doctor

Robert’s GP has an important task in acting as a gatekeeper for medical information when the patient himself has consulted dr. Google. It is important that the GP appears as a reliable source of guidance and advice for his patients. Self-diagnosis such as the one described here is an re-occurring situation. Practitioners must be critical in assessing symptoms and medical history to make accurate diagnoses and treatment plans, while also tending to building trust, listening to patients and addressing their concerns effectively.
Robert, a 45-year-old man, visits his GP. He explains that he has been experiencing symptoms of general fatigue and intermittent headaches over several months. Robert has made considerable efforts to understand his symptoms and their possible implications by conducting research online. To the consultation, he shows a lot of printed out material that describes potential diagnoses that align with his symptoms, some of which are severe conditions like Chronic Fatigue Syndrome, Lyme Disease, and brain tumors. Robert is worried about his health, asks the GP about what he is suffering from, and really wants a diagnosis. Based on the patient’s symptoms and medical history, it seems that Robert’s information isn’t correct and that he is not (seriously) ill.
Questions for reflection
- How can the GP approach Robert, who strongly believes in an incorrect diagnosis based on his online research, without causing unnecessary distress or infringing on their autonomy?
- How can the GP foster shared decision-making based on accurate information, thus promoting patient autonomy, empowerment, and beneficence in healthcare?
- How can the GP maintain an open dialogue with the patient about the information they find online while respecting their autonomy and dignity?
- What steps can the GP take to ensure that the patient does not feel overwhelmed or anxious due to their online health information findings going forward?